Lupus Foundation of America Statement on the Passing of Former Congresswoman Carrie P. Meek
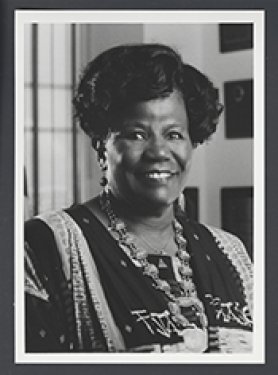
With saddened hearts, we share news of the passing of the Honorable Carrie P. Meek of Florida at age 95. Former Congresswoman Meek was a strong advocate for people with lupus, leading congressional efforts to secure funding for research and support services. She introduced and worked diligently to secure passage of the Lupus Research & Care Amendments Act of 2000. The legislation was co-sponsored by 258 members of Congress and signed into law on November 13, 2000, by President Clinton (Title V of Public Law 106-505).
The law authorized the U.S. Secretary of Health to expand research and related activities for lupus. These activities included coordinating services among federal agencies to address health disparities, increasing awareness to improve early diagnosis and treatment, and authorizing grants to federal, state, and local agencies and nonprofit organizations to expand healthcare and enhanced services for people with lupus.
Congresswoman Meek’s legislation stimulated federal agencies to expand their efforts on lupus. In 2002, for example, the U.S. Centers for Disease Control and Prevention (CDC) issued a landmark report showing deaths attributed to lupus had increased 70% between 1979 and 1998 among black women aged 45–64 years. Consequently, the CDC initiated strategies and funded research efforts, education programs, management activities and awareness campaigns to address health disparities in lupus.
The U.S. Department of Health (DHHS) Office on Women’s Health (OWH) initiated programs focused on improving early diagnosis and treatment among people at increased risk for lupus, including the first-of-its-kind National Ad Council campaign on lupus, “Could I have lupus?”
Other federal agencies followed OWH’s lead and stepped up their activities related to lupus, including the National Institutes of Health and the DHHS Office of Minority Health, which today continue to provide millions of dollars in federal funding for research, professional training, and public education programs and resources.
The Lupus Foundation of America, Board of Directors, and staff offer condolences to Congresswoman Meek’s family and colleagues and urge everyone with lupus to join us in expressing our sincere gratitude for her legacy of caring and support to our community.