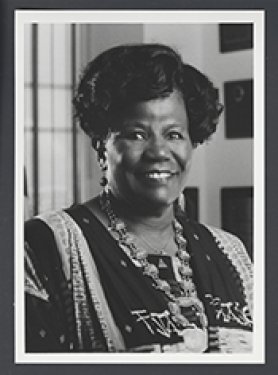
Bryant Reid Featured Speaker At The 100 Black Men of Atlanta Inc. Event
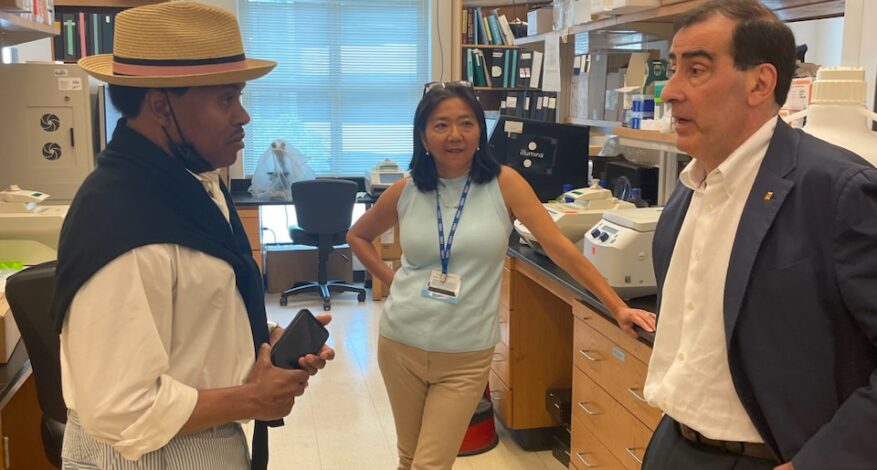
Bryant Reid, Founder and Board Chair, of The Reid Foundation for Lupus, Inc. (TRFL) was the featured speaker at the September 12, 2023, meeting of the General Body of the 100 Black Men of Atlanta Inc. Also, speaking at the event was Georgia Tech’s Men’s Head Basketball Coach Damon Stoudamire. The meeting was held in downtown Atlanta.
In his presentation, Mr. Reid spoke passionately about The Reid Foundation for Lupus, which he founded in 2018. He noted that lupus predominantly affects people of color. It, and those afflicted with this incurable disease, have not always received the support needed to provide relief to lupus victims. When Mr. Reid was diagnosed with the disease in 2009, he said he knew that he had to do something to help improve the quality of life for people living with lupus. The Reid Foundation for Lupus, Inc. was created out of this conviction.
The priorities of TRFL specifically include patient care programs, research, promotion of lupus awareness, grant-making to the Lupus Foundation of America’s Georgia Chapter and others. It will also include fundraising to support TRFL.

Mr. Reid also spoke about his success as a major behind-the-scenes figure in bringing about Atlanta’s status as a major cultural epicenter. He touched on ways he approached his major A&R responsibilities at LaFace Records. Highlights of this work included oversight of recording and/or remixes for the entire LaFace roster, including Toni Braxton, OutKast and TLC as well as his discovery of Usher Raymond.
He recounted memories of the night he found Usher at a talent show at Center Stage in Atlanta; how the LaFace A&R employee that he hired found the singer Pink; and the deal he secured which resulted in Donell Jones being signed at LaFace. Other highlights mentioned include his discovery of a young Jermaine Dupri, whom he hired to remix songs for Damian Dame; and TLC before his success with Kriss Kross. Mr. Reid concluded his remarks by discussing the reality-based music show he created in Atlanta on the Turner South Network back in 2002, a first of its kind.
The second speaker, Damon Stoudamire is currently the Head Coach for the Georgia Tech Yellow Jackets Men’s basketball program. He was the seventh overall pick by the Toronto Raptors in the 1995 NBA draft and won the NBA Rookie of the Year. Coach Stoudamire played collegiately at the University of Arizona and professionally for the Toronto Raptors, Portland Trail Blazers, Memphis Grizzlies, and San Antonio Spurs.
The meeting concluded with a reminder to the General Body of the mission of The 100 Black Men of Atlanta, which is to improve the quality of life by supporting and enhancing educational and economic opportunities, particularly for African-American youth in the Atlanta community.