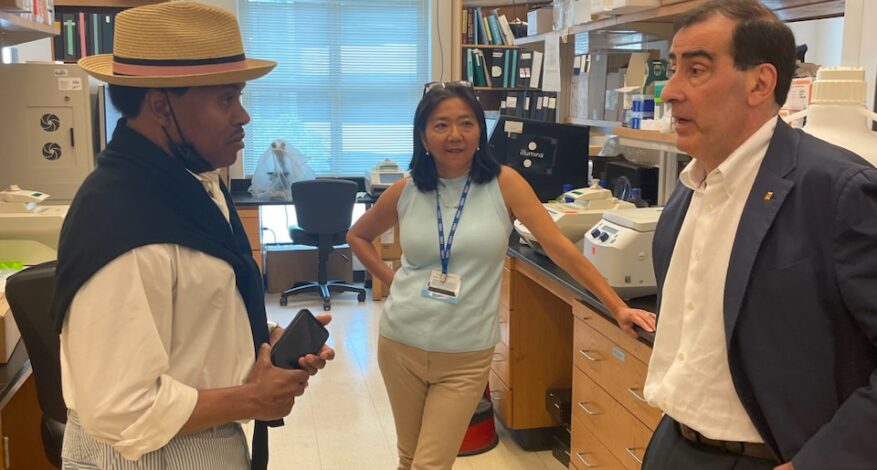
Bryant Reid Tours The Lowance Center For Human Immunology At Emory
Bryant Reid, The Reid Foundation For Lupus Chair, met with Dr. Ignacio Sanz, Emory Division of Rheumatology Director, and Dr. Frances Lee, Emory Department of Medicine Associate Professor at The Lowance Center for Human Immunology.
The purpose of the Lowance Center for Human Immunology is to understand the immunological and molecular mechanisms responsible for human autoimmune, inflammatory, and allergic diseases. The Lowance Center studies both the innate and adaptive arms of the immune response and the mutual regulation of the two components.

According to the Mayo Clinic, lupus is a disease that occurs when your body’s immune system attacks your own tissues and organs (autoimmune disease). Inflammation caused by lupus can affect many different body systems — including your joints, skin, kidneys, blood cells, brain, heart, and lungs. It most often affects people of color, African American, Hispanic, and Asian people.
The importance of the Lowance Center’s research in advancing the understanding of lupus is obvious. The purpose of Mr. Reid’s tour was to provide him with a more in-depth understanding of the scope of work at the Lowance Center and to discuss possible ways The Reid Foundation for Lupus could support or enhance their work.

Dr. Sanz and Dr. Lee provided Mr. Reid with fundamental insights into the depth and scope of lupus research at the Lowance Center. The high ethical standards and transparency of the research at the Center were apparent throughout the tour.
Mentioned was the outstanding work performed by the faculty and in particular Dr. Sam Lim, The Reid Foundation For Lupus Board Member, Drs; Khosroshahi and Williams. Despite its excellent reputation, the Lowrance Center still struggles to find participants to assist them in the research required to understand — or cure –the disease.
The Reid Foundation for Lupus could be an invaluable partner in assisting the Lowance Center in encouraging communities of color to participate in their lupus research studies.
Mr. Reid felt the tour was an important step in building a working relationship between The Reid Foundation for Lupus and other institutions at the forefront of finding effective treatments and, ultimately, a cure for lupus.